The following story was written by freelance writer Deborah Reid:
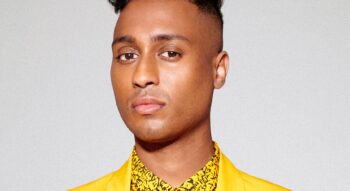
In his more than three decades of service, Kevin Smith, Chief of Niagara Emergency Medical Services and Director of Emergency Services Division, has prioritized community need. He’s curious and willing to evolve to suit the times. Early in his career, he set his sights on rising to a position where he could advocate for change. “I know anything is possible if I set my mind to it,” said Smith, who is an alumnus of Niagara College’s Ambulance and Emergency Care program from 1992.
Calm and charismatic, he was built for public service. As a young man, he took a year of radio and television broadcasting, and it’s evident in the way he communicates. That’s a prerequisite for a career that faces the public and includes oversight of 454 employees working 24/7 at many sites in the Niagara region.
He employs a journey metaphor when talking about the unique programs created under his leadership. Holding a vision over the long term and tracking achievements along the way are strengths.
Most of all, he has mastered the art of creating fruitful strategic partnerships.
The Mobile Integrative Health program has become a provincial model for a new type of emergency care, and it’s brimming with potential. When most people think of the job of a paramedic, they imagine a speeding ambulance with flashing lights and wailing sirens, but the reality is acute need accounts for about ten percent of 911 calls.
Over the years, there’s been a progressive and worrying pattern that’s put pressure on the system and the people working in it – emergency calls were nearing unmanageable proportions, and many of them didn’t qualify as acute.
So for ten years, from 2008 to 2018, Smith methodically began testing new delivery systems, hoping they would lead to impactful results. Most of this was happening while he was undertaking advanced studies. It’s remarkable to think that Smith felt insecure about his ability to succeed in school as a young man.
Research and analysis made it clear that the greatest need was among seniors waiting for long-term care. And many of their calls were about mental health issues or falls. Applying an interdisciplinary approach to problem-solving, Smith began partnering paramedics with a mental health practitioner or an occupational therapist.
At the same time, the nature of the process became preventative. Instead of waiting for the call, they went into the community to assess the needs of frequent callers and connect them with the right resources. They also began a pilot program that put a nurse in dispatch to triage calls that weren’t acute.
What was being done in the Niagara region was unique. “Because no one was doing this in North America, we formed a partnership in Wales with the Welsh Ambulance Service Trust,” said Smith. “We did exchanges and discovered a lot of similarities in our approach and the services we were offering.”
There are many partnership opportunities, but Smith has had to turn down resource providers for capacity reasons and because it’s still early days. New programs and specialized training for paramedics are ongoing. Palliative care and supervised consumption sites are two areas that also put pressure on emergency care services.
An advocate for evidence-informed decision-making led to partnerships with academic institutions. Working with a research team from McMaster University, a study was done to examine the economic impact of the Mobile Integrated Health model. In February 2021, the findings were published in the prestigious Journal of the American Medical Association.
Having the program in place before the COVID-19 crisis was advantageous in expediting public health messaging and dealing with practical matters like hospital transfers.
This year, the provincial government made an 8.2-million-dollar investment in the Mobile Integrated Health program. Time will tell if they replicate the program in communities throughout Ontario, or if it is a stop-gap measure until home health-care resources are strengthened.
“The work we are doing here is being watched very closely by the province,” said Smith. “We’re a model.”
This story is part of a series featuring seven distinguished members of Niagara College’s alumni community, who have been nominated for Colleges Ontario’s prestigious 2021 Premier’s Awards.